Surgical fixation versus conservative management for rib fractures caused by blunt chest trauma: a comparative study
Published: 15 October 2025
Volume 4Abstract
Rib fractures are a frequent consequence of blunt chest trauma and are associated with significant morbidity and mortality, particularly in cases of flail chest or multiple displaced fractures. While conservative management remains the traditional approach, surgical stabilization of rib fractures (SSRFs) has gained increasing attention for its potential to improve outcomes. This prospective comparative cohort study, conducted between April 2018 and August 2023, compared the effectiveness of SSRF with that of nonoperative management. A total of 114 patients with respiratory compromise from unstable rib fractures were enrolled, 57 of whom underwent SSRF via custom-made titanium plates and screws (Group A) and 57 of whom received conservative treatment (Group B). Baseline demographics and associated injuries were comparable between the groups, although flail chest was more common in the surgical cohort (40.4% vs. 19.3%, p = 0.012). By discharge, patients in the SSRF group reported significantly lower pain scores (3.6 vs. 7.5, p < 0.001) and demonstrated superior pulmonary function at follow-up (FEV₁ at 3 months: 2.84 ± 0.40 L vs. 2.06 ± 0.36 L, p < 0.001). Oxygen dependence was shorter in the surgical group (2.5 ± 0.7 vs. 5.1 ± 0.8 days, p < 0.001), and fewer patients required ventilatory support (12.3% vs. 29.8%, p = 0.022). Among ventilated patients, 50% in the SSRF group were weaned within 3 days, whereas none were weaned in the conservative group (p < 0.001). The length of hospital stay was nearly halved with surgery (4.4 ± 1.5 vs. 9.4 ± 2.3 days, p < 0.001). Mortality was lower in the surgical group (5.3% vs. 15.8%), although this difference was not statistically significant (p = 0.062). Importantly, return-to-work rates at one month were markedly higher following SSRF (62.96% vs. 12.50%, p < 0.001). Compared with conservative management, SSRF offers significant benefits in terms of pain control, respiratory recovery, and functional outcomes. These findings support broader adoption of SSRF, particularly in patients with flail chest or multiple displaced rib fractures, and highlight the feasibility of custom-made implants in resource-limited settings.
Keywords
Rib fractures; Fracture fixation, internal; Thoracic injuries; Conservative treatment; Treatment outcome
1. Introduction
Thoracic trauma frequently leads to rib fractures, which are often accompanied by damage to the pleura, intrathoracic vessels, and pulmonary parenchyma. These injuries can lead to serious complications, such as pulmonary contusions, hemothorax, pneumothorax, and diaphragmatic trauma. When rib fractures are accompanied by a flail chest segment, the risk of respiratory compromise significantly increases, often necessitating ventilatory support and contributing to higher morbidity and mortality rates [1,2,3,4].
Compared with isolated and multiple nonflail rib fractures, flail chest fractures are associated with poorer outcomes because of their increased occurrence of respiratory insufficiency and concurrent injuries [5,6]. Traditionally, rib fractures are managed conservatively with respiratory support, analgesia, and physiotherapy. Although surgical stabilization of rib fractures (SSRFs)—historically referred to as surgical fixation—was first described in the early 20th century, it remained uncommon until recent advances in surgical techniques, implant technology, and thoracic surgical expertise.
Several recent studies have compared SSRF with conservative approaches in the management of rib fractures, particularly those presenting with flail chest [6]. These studies consistently demonstrated that, compared with nonoperative treatment, SSRF significantly reduces the duration of mechanical ventilation, ICU and hospital stays, incidence of pneumonia, and need for tracheostomy [7,8].
Despite these benefits, surgical intervention is still underutilized in many centers because of variability in clinical guidelines, the limited availability of surgical expertise, and concerns about operative risks. Consequently, real-world data comparing the two approaches in different trauma populations are crucial for optimizing patient selection and outcomes. Therefore, this research aimed to evaluate the clinical outcomes of SSRF compared with those of conservative management in patients with flail chest fractures or multiple displaced rib fractures. We hypothesized that operative fixation, when applied under appropriate indications and performed by experienced surgeons, would yield superior short- and medium-term outcomes and inform best practices in rib fracture management.
2. Methodology
2.1. Study design and setting
This prospective, comparative cohort study was conducted at the Department of Thoracic Surgery, Combined Military Hospital (CMH), Rawalpindi, between April 2018 and August 2024.
2.2. Selection criteria
Patients aged ≥ 16 years who presented with respiratory compromise due to painful, unstable rib fractures refractory to analgesia were considered for inclusion. Eligible cases included individuals with flail chest, multiple (≥ 4) severely displaced rib fractures, or thoracic injuries requiring thoracotomy. Patients were excluded if they had severe head or spinal injuries; polytrauma with multiorgan failure (MOF); acute respiratory distress syndrome (ARDS); empyema; or significant systemic diseases such as advanced cardiac, hepatic, or renal dysfunction.
2.3. Sample size
The sample size was based on Liu et al. [9], who reported mean ICU stays of 4.02 ± 1.41 days after surgery versus 5.06 ± 1.80 days with conservative care. Using these values, with a pooled standard deviation of 1.615, a two-tailed α of 0.05, and 80% power, the minimum required sample size was estimated to be 38 patients per group via the online sample size calculator ClinicCal [10]. To strengthen the analysis and allow for detailed subgroup comparisons, a total of 57 patients were enrolled per group.
2.4. Study groups and interventions
A total of 114 patients meeting the criteria were enrolled via convenience sampling and divided into two equal groups. Group A (n = 57) underwent SSRF via titanium locking plates (1.9 mm thickness, 10 mm width) and 3.5 mm locking screws. All procedures were performed by experienced thoracic surgeons under general anesthesia. Group B (n = 57) received conservative treatment consisting of multimodal analgesia (oral, intravenous, or epidural), oxygen therapy, nebulization, and chest physiotherapy.
2.5. Follow-up and outcome measures
A three-month follow-up was completed for all patients, with assessments at 1, 2, and 3 months post-treatment. The outcomes evaluated included pain severity via the VAS, pulmonary function measured via spirometry (FEV1), and radiographic assessment of rib healing. Additional parameters included hospital and ICU stay duration, oxygen dependence, need for ventilatory support and duration of weaning, incidence of pulmonary infection, mortality, and return-to-work status. Associated injuries such as hemothorax, pneumothorax, flail chest, clavicle fractures, and diaphragmatic injury were also documented.
2.6. Ethical approval
The study was approved by the Institutional Review Board of the CMH, Rawalpindi (No. 815). All participants provided written informed consent.
2.7. Statistical analysis
Statistical analysis was performed using IBM SPSS version 26. The data were analyzed as the means with standard deviations, frequencies, and percentages. Group comparisons were conducted with the Mann–Whitney U test, chi-square test, and Fisher’s exact test. A p value < 0.05 was considered statistically significant.
3. Results
Table 1 shows the baseline demographic and injury-related characteristics of the patients in both groups. The distributions of sex, hemothorax, pneumothorax, bilateral rib fractures, clavicle fractures, and diaphragmatic injuries were statistically comparable between the groups (p > 0.05 for all). However, flail chest was significantly more common in the SSRF group, affecting 40.4% of patients, whereas it affected 19.3% of patients in the conservative group (p = 0.012). While hemothorax and pneumothorax were slightly more common in the SSRF group (91.2% and 89.5%, respectively), these differences were not statistically significant. Diaphragmatic injury was observed only in the SSRF group (3.5%) but occurred rarely overall.
| Variables | Group A: Surgical (n = 57) |
Group B: Conservative (n = 57) |
p Value | |
| Frequency (%) | Frequency (%) | |||
| Sex | Male | 39 (68.4) | 33 (57.9) | 0.244 |
| Female | 18 (31.6) | 24 (42.1) | ||
| Hemothorax | 52 (91.2) | 46 (80.7) | 0.106 | |
| Pneumothorax | 51 (89.5) | 53 (93.0) | 0.508 | |
| Bilateral rib fracture | 8 (14.0) | 9 (15.8) | 0.793 | |
| Flail chest | 23 (40.4) | 11 (19.3) | 0.012 ** | |
| Clavicle fracture | 9 (15.8) | 7 (12.3) | 0.59 | |
| Diaphragmatic injury | 2 (3.5) | 0 (0.0) | 0.496 | |
| * Data were analyzed via the chi-square test and Fisher’s exact test. ** Significance at p < 0.05. | ||||
Table 2 compares the clinical outcomes between the two groups across pain scores, lung function (FEV1), and oxygen dependence. The initial pain scores at admission were similar (p = 0.416), indicating comparable baseline discomfort. By discharge, however, patients who underwent SSRF reported significantly lower pain scores, averaging 3.6 vs. 7.5 in the conservative group (p < 0.001). In addition, the analgesic requirements differed: patients in the SSRF group were managed with on-demand oral or epidural analgesia, whereas those in the conservative group required continuous multimodal analgesia for approximately three days. Pulmonary function, as measured by FEV1, was consistently greater in the SSRF group than in the control group at all follow-up intervals. At three months, the mean FEV1 reached 2.84 L in the SSRF group compared with 2.06 L in the conservative group, reflecting a 38% greater volume (p < 0.001). The need for supplemental oxygen was also significantly lower among surgically treated patients, who required support for an average of 2.5 days versus over 5 days in the conservative group (p < 0.001), demonstrating faster respiratory recovery.
| Variables | Group A: Surgical (n = 57) |
Group B: Conservative (n = 57) |
p Value |
| Mean ± SD | Mean ± SD | ||
| Pain Score at admission | 8.544 ± 0.569 | 8.632 ± 0.522 | 0.416 |
| Pain score at discharge | 3.579 ± 1.209 | 7.526 ± 1.754 | < 0.001 ** |
| FEV1 at 1 month (L) | 2.062 ± 0.137 | 1.534 ± 0.310 | < 0.001 ** |
| FEV1 at 2 months (L) | 2.597 ± 0.440 | 1.859 ± 0.317 | < 0.001 ** |
| FEV1 at 3 months (L) | 2.838 ± 0.400 | 2.056 ± 0.358 | < 0.001 ** |
| Oxygen dependence (in days) | 2.509 ± 0.710 | 5.140 ± 0.833 | < 0.001 ** |
| * Data were analyzed via the Mann–Whitney U test. ** Significance at p < 0.05. | |||
Table 3 highlights significant differences in ventilatory needs and hospital course. Ventilatory support was required in 12.3% of the SSRF patients compared with 29.8% in the conservative group (p = 0.022). Among ventilated patients, half of those in the SSRF group were weaned within 3 days, whereas no patient in the conservative group achieved early weaning. The majority of conservatively managed patients (70.6%) required prolonged ventilation beyond 5 days (p < 0.001). The mean hospital stay was markedly shorter in the SSRF group (4.4 ± 1.5 days) than in the conservative group (9.4 ± 2.3 days) (p < 0.001). Although mortality was lower in the SSRF group (5.3% vs. 15.8%), this difference did not reach statistical significance (p = 0.062).
| Variables | Group A: Surgical | Group B: Conservative | p Value | |
| Frequency (%) | Frequency (%) | |||
| Ventilatory support | 7 (12.3) | 17 (29.8) | 0.022 *** | |
| Weaning from ventilator | Weaning < 3 days | 4 (50.00) | 0 (0.0) | < 0.001 *** |
| Weaning 3–5 days | 4 (50.00) | 5 (29.4) | ||
| Weaning > 5 days | 0 (0.0) | 12 (70.6) | ||
| Mean hospital stay (days ± SD) | 4.421 ± 1.499 | 9.421 ± 2.322 | < 0.001 *** | |
| Mortality | 3 (5.3) | 9 (15.8) | 0.062 | |
| * Data were analyzed via the chi-square test, Fisher’s exact test, or the Mann–Whitney U test. ** Duration of weaning categorized by intervals. *** Significance at p < 0.05. | ||||
Table 4 shows the return-to-work outcomes across the follow-up intervals. A significantly greater proportion of SSRF patients had resumed work by one month (62.96% vs. 12.50%, p < 0.001). At two months, the return-to-work rates increased in both groups (27.78% in the SSRF group vs. 41.67% in the conservative group). By three months, 100% of the SSRF patients had resumed work, whereas 77.09% had resumed work in the conservative group, indicating faster and more complete functional recovery with surgical management.
| Variables | Group A: Surgical (n = 54) |
Group B: Conservative (n = 48) |
p Value | |
| Frequency (%) | Frequency (%) | |||
| Return to work status | At 1 month | 34 (62.96) | 6 (12.50) | < 0.001 *** |
| At 2 months | 15 (27.78) | 20 (41.67) | ||
| At 3 months | 5 (9.26) | 11 (22.92) | ||
| * Return-to-work frequencies were calculated among surviving patients and compared via the chi-square test. ** At 3 months, 11 patients (22.92%) in Group B had not returned to work. *** Significance at p < 0.05. | ||||
Preoperative imaging (Figure 1) provided detailed 3D CT reconstructions of rib fractures, assisting in surgical planning. Intraoperative photographs (Figure 2) illustrate the exposure, reduction, and fixation of fractures with titanium plates and screws, demonstrating the technical feasibility of SSRF. Postoperative radiographs (Figure 3) confirmed satisfactory alignment and secure fixation, which was consistent with the improved clinical outcomes observed in the SSRF group.
Figure 1. Three-dimensional computed tomography (CT) reconstruction of the thoracic cage demonstrating multiple displaced rib fractures predominantly involving the left lateral and posterolateral ribs. This scan was used preoperatively for fracture assessment and surgical planning.
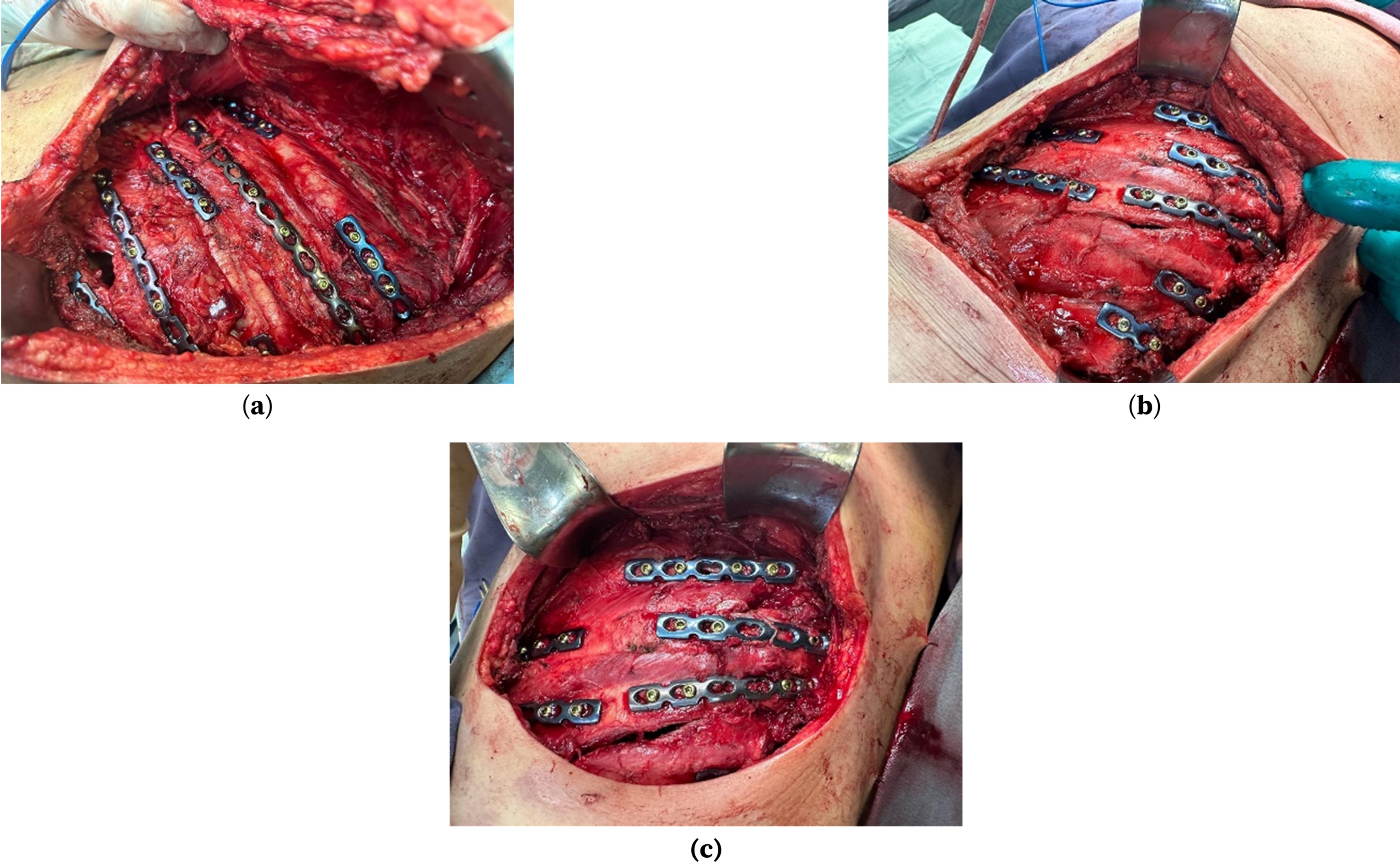
Figure 2. Intraoperative images showing surgical rib fixation via titanium locking plates and screws. (a) Exposure of multiple displaced rib fractures prior to fixation. (b) Alignment and plating of fractured segments. (c) Final view after complete fixation and stabilization of the ribs.
Figure 3. Postoperative chest X-ray image showing stable alignment of the ribs with visible titanium plates on the right side of the thoracic cage, confirming successful surgical fixation.
4. Discussion
This study demonstrated that the SSRF offers meaningful clinical benefits over nonoperative management in adult patients with multiple rib fractures following blunt chest trauma. Patients in the surgical group experienced significantly shorter hospital stays, reduced oxygen dependence, and improved pulmonary function recovery. These findings support the growing body of evidence favoring operative fixation in carefully selected patients with unstable chest wall injuries [11,12].
The observed benefits are attributed primarily to biomechanical stabilization of the thoracic cage, which improves pulmonary mechanics, reduces paradoxical chest movement, and enhances pain control, as evidenced by our lower discharge VAS scores (3.6 vs. 7.5). Similar improvements in pain relief with surgical fixation have been reported by Majeed et al., who reported a significant reduction in postoperative pain compared with conservative management (VAS 3.6 vs. 5.5, p = 0.032) [13]. This enhanced stabilization facilitates improved pulmonary hygiene, earlier ambulation, and accelerated respiratory recovery, as reflected in our superior FEV₁ values at 1, 2, and 3 months post-injury. These outcomes are consistent with prior evidence demonstrating the role of SSRF in optimizing pulmonary function recovery [14,15].
In addition, the surgical cohort in our study required significantly less ventilatory support, was weaned earlier, and demonstrated a trend toward lower in-hospital mortality than did the nonoperative cohort. These results align with those of the meta-analysis by Leinicke et al., which revealed that, compared with conservative management, surgical stabilization reduced the duration of ventilator use by an average of 4.5 days; shortened the ICU stay by 3.4 days and hospital stay by 5 days; and significantly lowered the risks of pneumonia, tracheostomy, and mortality [16].
However, our results contrast with those of Meyer et al., who, in a randomized controlled trial of severe chest wall injury without clinical flail chest, reported a significantly longer hospital stay in surgically managed patients (median 9 days) than in those treated conservatively (median 6 days) [17]. While some studies have similarly reported longer ICU or hospital stays among surgically treated patients, these findings are often attributable to differences in baseline injury severity. In particular, a greater proportion of flail chest cases in the operative groups—as observed in our cohort (23 vs. 11 cases)—likely contributed to the increased resource utilization in those studies [18].
Another important factor is patient selection bias inherent in nonrandomized studies, where patients with more severe injuries are frequently allocated to surgical intervention. This may partly explain the variability in reported outcomes across the literature and emphasize the importance of context-specific interpretation of results [19].
In the context of low-resource settings, the adoption of custom-made, low-cost rib fixation implants has been associated with favorable clinical outcomes and a significantly faster return to work [19,20]. In our study, all surgically treated patients had resumed employment by three months, compared with only 77.09% in the conservative group. These results highlight not only the clinical benefits of SSRF but also its potential long-term economic and functional advantages, particularly in resource-limited healthcare settings [19].
Our findings also align with several recent meta-analyses, including a comprehensive review in 2022, which concluded that SSRF reduces mortality, pneumonia, and duration of mechanical ventilation—particularly in patients with flail chests [19,20]. These analyses also emphasize the importance of early surgical intervention, with Sawyer et al. demonstrating that procedures performed within 72 hours were associated with significantly improved outcomes, including shorter hospital and ICU stays, lower pneumonia rates, and fewer deaths [21].
Finally, beyond short-term recovery, surgical fixation restores thoracic symmetry, corrects deformities, and prevents nonunion—factors that are crucial for preserving long-term pulmonary function and optimizing physical recovery [22,23]. While some reports suggest comparable pain outcomes between operative and nonoperative groups [24,25], our data indicate a superior quality of recovery with surgical intervention, as evidenced by lower discharge VAS scores and improved pulmonary function over follow-up. These discrepancies are likely explained by patient selection bias in nonrandomized studies [26].
As this was a single-center study, our results may not be generalizable to other public or private institutions with different patient populations, socioeconomic backgrounds, or levels of surgical expertise. Variability in operative technique and implant selection could also influence outcomes, and nonuniform follow-up durations may have limited the accuracy of assessing chronic pain, nonunion, or long-term functional recovery [27]. Although efforts have been made to control for confounding factors, such as the uneven distribution of flail chest cases, selection bias remains an inherent limitation. While propensity score matching and careful statistical adjustment can reduce this effect, they cannot substitute for the rigor of randomized controlled trials. In addition, excluding deceased patients from functional outcomes such as return-to-work may introduce survivor bias, potentially overestimating recovery in the conservative group, where mortality was higher. The reliance on scheduled follow-up rather than real-time monitoring may also have introduced recall or reporting bias in outcomes such as return-to-work or pain scores. Future research should therefore focus on large, multicenter RCTs to validate the benefits of rib fixation in both flail and nonflail fracture patterns, complemented by rigorous cost-effectiveness analyses to better define the economic implications of surgical stabilization. Additionally, the development of standardized treatment protocols—including clear indications, optimal timing of fixation, implant choice, and postoperative rehabilitation—will help reduce variability in practice. Finally, incorporating patient-reported outcomes, such as pain, quality of life, and return-to-work measures, will provide a more holistic evaluation of treatment success and its impact on long-term recovery [28].
5. Conclusions
Compared with conservative management, SSRF in appropriately selected patients with flail chest fractures or multiple displaced rib fractures demonstrated clear clinical benefits in this study. Operative fixation resulted in significantly better pain control, improved pulmonary function recovery, shorter hospital stays, earlier return to work, and reduced ventilatory support requirements. Although a trend toward lower mortality was observed in the surgical group, this difference did not reach statistical significance. The successful use of custom-made, low-cost implants further highlights the feasibility and value of SSRF in resource-limited settings. Conservative treatment remains an appropriate option for nondisplaced injuries or patients who are unfit for surgery and who are provided with optimal analgesia and pulmonary care.
Author contributions
Conceptualization, FAM; methodology, FAM, AR, and ARA; software, AR, FU, and ARA; validation, FAM, and RM; formal analysis, FAM, AR, RM, ARA, and SC; investigation, FU; resources, RM, and SC; data curation, FAM, and FU; writing—original draft preparation, FAM; writing—review and editing, AR, RM, FU, ARA, and SC; visualization, SC; supervision, FAM; project administration, FAM. All authors have read and agreed to the published version of the manuscript.
Publication history
| Received | Revised | Accepted | Published |
| 09 July 2025 | 04 September 2025 | 07 September 2025 | 15 October 2025 |
Funding
This research received no specific grant from the public, commercial, or not-for-profit funding agencies.
Ethics statement
The study was approved by the Institutional Review Board of the CMH, Rawalpindi (No. 815).
Consent to participate
Not applicable.
Data availability
The data supporting this study's findings are available from the corresponding author, Ahmed Raza, upon reasonable request.
Acknowledgments
None.
Conflicts of interest
The authors declare no conflicts of interest.
Copyright
© 2025 The Author(s). This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY) License. The use, distribution, or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Publisher's note
Logixs Journals remains neutral concerning jurisdictional claims in its published subject matter, including maps and institutional affiliations.
References
Apampa AA, Ali A, Kadir B, Ahmed Z. Safety and effectiveness of surgical fixation versus non-surgical methods for the treatment of flail chest in adult populations: a systematic review and meta-analysis. EurEur J Trauma Emerg Surg. 2022;48:1025-34. https://doi.org/10.1007/s00068-021-01606-2
Dai NV, Son PDH, Tu VN, Anh NV, May NT, Duy VK, et al. Comparison of in-hospital outcomes of surgical stabilization of rib fractures with nonsurgical management: a multicenter, prospective, cohort study. Acta Inform Med. 2023;31(4):275-9. https://doi.org/10.5455/aim.2023.31.275-279
ClinCalc.com. Sample size calculator. 2025 [cited 13 October 2025]. Available from: https://clincalc.com/stats/samplesize.aspx.
Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52(4):727-32. https://doi.org/10.1097/00005373-200204000-00020
Jensen CD. The treatment of rib fractures with thoracic epidural analgesia [dissertation]. Storrs (CT): University of Connecticut; 2015.
Wijffels MME, Hagenaars T, Latifi D, Van Lieshout EMM, Verhofstad MHJ. Early results after operatively versus non-operatively treated flail chest: a retrospective study focusing on outcome and complications. Eur J Trauma Emerg Surg. 2020;46:539-47. https://doi.org/10.1007/s00068-018-0961-4
Perentes JY, Christodoulou M, Abdelnour-Berchtold E, Karenovics W, Gayet-Ageron A, Gonzalez M, et al. Effectiveness of rib fixation compared to pain medication alone on pain control in patients with uncomplicated rib fractures: study protocol of a pragmatic multicenter randomized controlled trial—the PAROS study (Pain After Rib OSteosynthesis). Trials. 2022;23:732. https://doi.org/10.1186/s13063-022-06509-0
Cruz-De La Rosa KX, Ramos-Meléndez EO, Ruiz-Medina PE, Arrieta-Alicea A, Guerrios-Rivera L, Rodríguez-Ortiz P. Surgical rib fixation is associated with lower mortality in patients with traumatic rib fractures. J Surg Res. 2024;295:647-54. https://doi.org/10.1016/j.jss.2023.11.046
Fagevik Olsén M, Slobo M, Klarin L, Caragounis EC, Pazooki D, Granhed H. Physical function and pain after surgical or conservative management of multiple rib fractures – a follow-up study. Scand J Trauma Resusc Emerg Med. 2016;24:128. https://doi.org/10.1186/s13049-016-0322-4




